VISBY MEDICAL™ PATIENT CASE STUDY
A case of overtreatment associated with syndromic management of STIs
Case Study #1: Hannah

This study is based on a real-life case.1 Some details have been altered to fit the format of this study to preserve the identity of the patient. All photos are stock photos, used for illustrative purposes only. Posed by models.
Case Intro
Day 1 (Clinic Visit): Meet Hannah
Hannah, an 18-year-old female college freshman, presents to the local clinic with a week-long history of vaginal discharge and itching.
Did you know?
Tina: Vaginal discharge, which is comprised of skin cells, bacteria, mucus, and fluid, helps protect the lower female reproductive tract and urinary tract by providing lubrication to the vaginal tissue and protecting against infections. Premenopausal women produce approximately 1/2 to 1 teaspoon (2-5 mL) of vaginal discharge each day. Discharge can be a completely normal finding in women, specifically if it is white or clear, thick, mucus-like, and odorless.2 However, when vaginal discharge presents with any of the following signs and symptoms, it’s abnormal and should be evaluated by a medical professional.2
- Itching of the vulva or vagina
- Redness, burning, swelling of vulva
- Discharge that is odorous, foamy, green/yellow colored, and/or bloody
- Abdominal or pelvic pain
Case Update
Day 1 (Clinic Visit): Medical and Sexual History
In the exam room, the nurse collects medical and sexual history, including more information about Hannah’s chief complaint.
- Vaginal discharge and itching
- No abdominal or pelvic pain
- No other notable symptoms
Hannah shares that she has a new sexual partner. The nurse indicates that a urine sample is needed to ensure that Hannah is not pregnant and to conduct a urinalysis to screen for a potential urinary tract infection (UTI), which may also present with symptoms similar to those of sexually transmitted infections (STIs)
Nurse-patient dialogue
Nurse: When did the discharge and itching start and how would you describe it?
Hannah: It all started several days ago. The discharge is more than what I usually have and is white-ish. The itchiness is something that I have never experienced before.
Nurse: Are you sexually active? If so, do you have any new sexual partners?4
Hannah: Yes, I broke up with my first partner a few months ago and I have since started seeing someone new. Our relationship turned into a sexual relationship a few weeks ago.
Nurse: If you use pregnancy and STI prevention methods, which ones do you use (e.g., condoms, oral contraceptives like birth control pills) and how often do you use them?3
Hannah: I’m on birth control pills, and although I take one every day, I sometimes forget to take it until bedtime when I usually take it first thing in the morning.7 Typically, my partner uses a condom, but there were a few times when we didn’t use one.

Quiz Question #1
Case Update
Day 1 (Clinic Visit): Physical and Pelvic Exams, Lab Assessments
Hannah collects the urine sample for in-house processing and prepares for the physical and pelvic exam by the physician.4
Examinations10
Physical Exam
- All vitals are within normal limits
- Patient is alert, well-developed, and well-nourished and appears to not be in acute distress; however, she does seem to be slightly nervous or upset.
Pelvic Examination
External findings:
- Noted slight erythema, or redness, of the vulva. Patient confirms that this is consistent with the location of the itching.
Internal findings:
- Cervix appears unremarkable; no mucopurulent cervicitis (MPC) is noted.
- White discharge is present in the vaginal canal.

Laboratory Assessments
Vaginal swab is collected for lab analysis
External lab assessments1,11
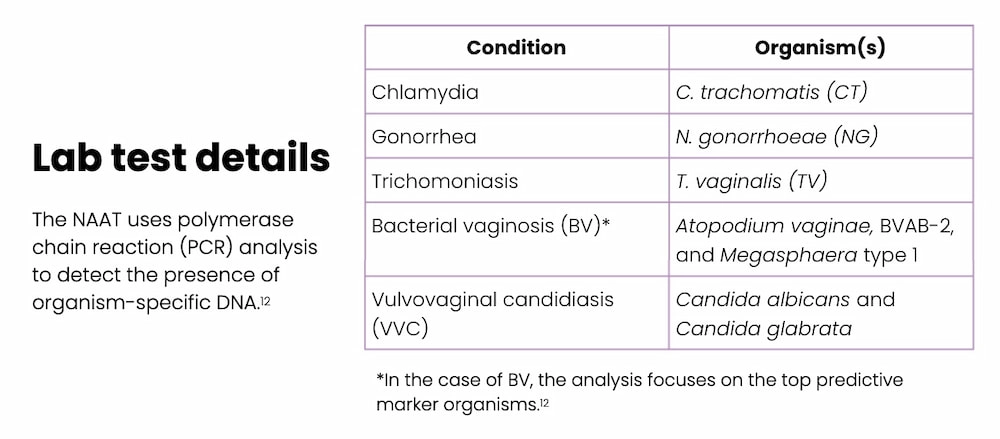
- Vaginal swab is sent to an external lab for a nucleic acid amplification test (NAAT) to detect the presence of organisms that can cause conditions suspected in the differential diagnosis, including the most common causes of abnormal vaginal discharge — chlamydia, gonorrhea, trichomoniasis, and VVC1, 11
In-house urine assessment
- Human chorionic gonadotropin (hCG): not detected, negative.
- Visual assessment: clear, straw-colored
- Chemistry assessment: no protein, glucose, or blood detected
Did you know?
According to the World Health Organization (WHO) Guidelines for the Management of Symptomatic STIs, all women who present with abnormal vaginal discharge should undergo a comprehensive medical and sexual history in addition to a physical exam, which should include a pelvic exam using a speculum to visualize the cervix
Quiz Question #2
Case Update
Day 1 (Clinic Visit): Treatment Plan4
The physician reviews Hannah’s case notes.
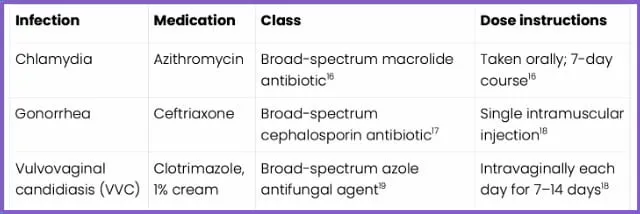
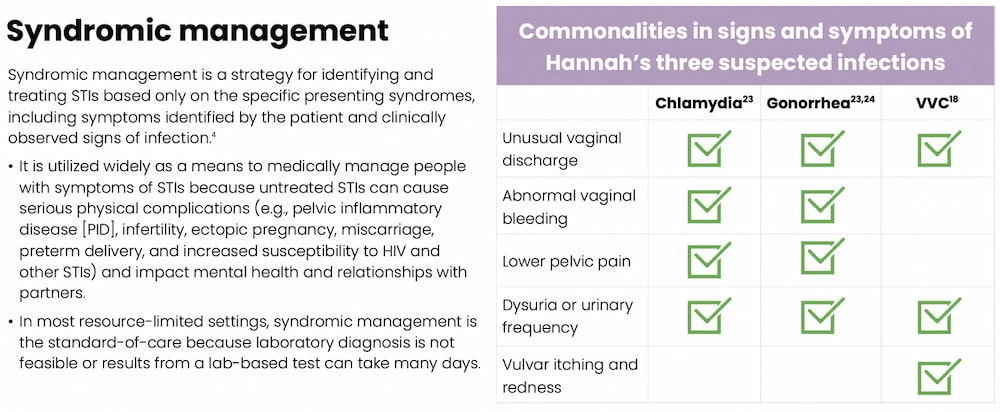
A definitive diagnosis from the lab test will likely not be available for several days, so the physician recommends presumptive treatment or syndromic management targeting the following three potential infections

Did you know?
Urinary symptoms are associated with both UTIs and STIs, and both infections can occur concomitantly. It is estimated that about 20% of adult females with a culture-confirmed UTI also have a concomitant vaginal or cervical infection caused by an SI, including chlamydia, gonorrhea, and trichomoniasis.6
In a study of 296 sexually active females (aged 14-22 years), patients presenting with urinary symptoms in the absence of a formal UTI diagnosis, were more likely to have a trichomoniasis infection than a UTI. Additionally, 65% of patients presenting with sterile pyuria, actually had an STI, specifically trichomoniasis or gonorrhea. This makes it challenging for clinicians to determine if the origins of urinary symptoms are in fact due to a UTI or if they may be the result of an STI.6
Quiz Question #3
Case Update
Day 4
The clinic receives STI lab results, which have been reviewed by the physician, and they confirm that Hannah does not have any of the STIs or other infections that were suspected (i.e., chlamydia, gonorrhea, or VVC), nor did she have BV or trichomoniasis.

Case Update
Day 5
The clinic attempts to contact Hannah several times before reaching her to inform her of the lab results. Hannah is instructed to discontinue treatment.
At this point, Hannah has had an intramuscular injection of ceftriaxone, a course of azithromycin, and five daily applications of intravaginal clotrimazole; all of which were not medically necessary in light of the lab results. The physician suspects a noninfectious cause and asks Hannah to schedule a follow-up appointment if symptoms persist.4
Key Point
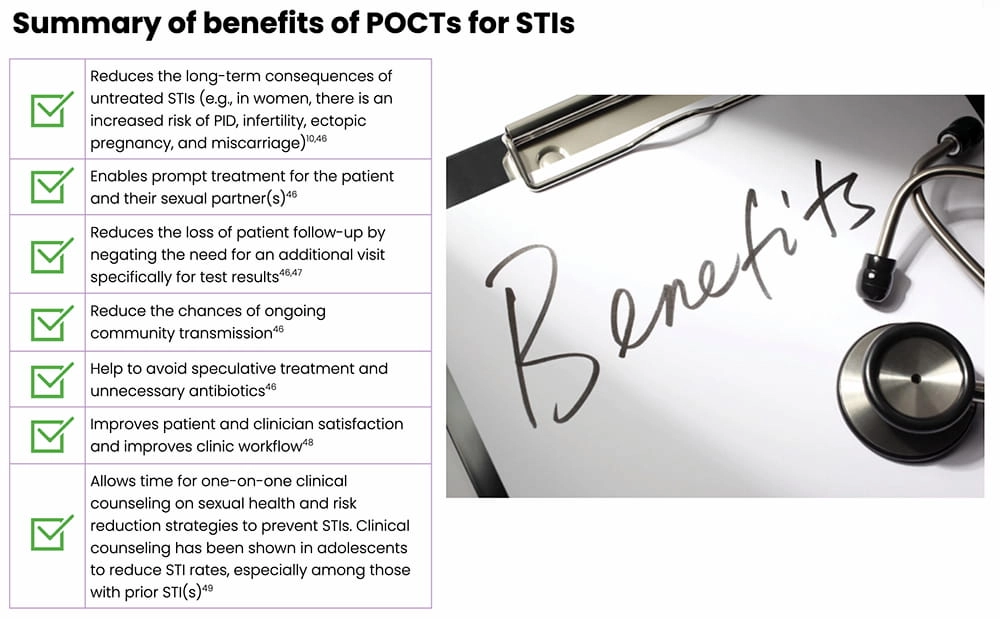
Under syndromic management, the WHO reports that there is considerable overtreatment of women presenting with vaginal discharge with antibiotics. Simple, rapid, and accurate Point-of-Care tests (POCTs) can greatly improve STI management by allowing a clinician to definitively diagnose and appropriately treat potential STIs.28,29
Implications of Undertreatment
Inappropriate antibiotic use
- There is a global surge in antibiotic resistance among bacterial STIs, especially gonorrhea, resulting in limited effective treatment options.4 In fact, over time, gonorrhea has developed resistance to almost all antibiotics that have been used to treat it.30

- Antibiotics, like all medications, come with side effects, including rash, dizziness, nausea, diarrhea, and increased risks of yeast and Clostridioides difficile (C. diff.) infections. According to the Centers for Disease Control and Prevention (CDC), adverse reactions associated with antibiotic use account for 1 out of 5 medication-related visits to the emergency room.31
- Antibiotic use has been shown to alter the vaginal flora, specifically resulting in the loss of the protective Lactobacillus strains.32 Normally, lactobacilli help maintain an acidic environment to promote their own growth and also help to ward off harmful microbes and viruses by releasing antimicrobial- and viricidal-like compounds.32,33 The loss of Lactobacillus strains following antibiotic treatment can result in a less acidic environment that is increasingly susceptible to infections like BV, VVC, and UTIs.32,34
Costs
- There are costs associated with medications and treating any subsequent bacterial infections that develop resistance to current recommended therapies (e.g., medical care to address comorbidities and receive additional treatments).4
- Also, there are costs related to the research and development needed to produce novel antibiotic therapies to address the surge in resistance.4
Mental effects
- Patients treated for or diagnosed with an STI may experience shame, embarrassment, negative stigma, and loss of self-worth.1,4
Case Update
What if STI Test Results Are Available During the Clinic Visit?
Let’s revisit Hannah’s story but see how differently it would go if the clinic was equipped with a rapid, highly accurate POCT, such as the Visby Medical Sexual Health Test…
- During her clinic visit, the nurse asks Hannah to provide a self-collected vaginal swab and urine sample; both samples are processed right away, at the start of the visit.
30 minutes later…1
- Hannah meets with the physician who has both her urinalysis and the POCT results.
- The POCT revealed that Hannah does not have chlamydia, gonorrhea, or trichomoniasis

Key Point
If this POCT had been used in the clinic, Hannah would not have received treatment for chlamydia and gonorrhea under a syndromic management protocol.4
Note: Detection of organisms that cause BV and VVC are not part of the Visby Medical Sexual Health Test; an alternate diagnostic test would be needed for those two infections.
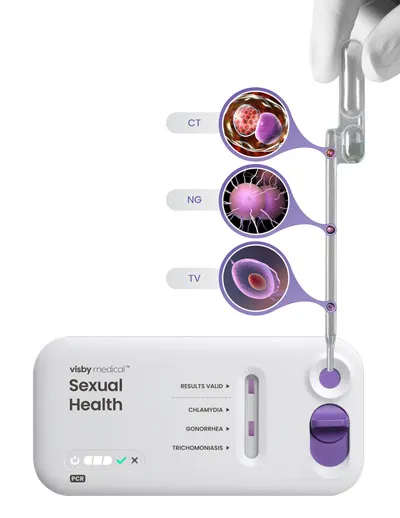
Visby Medical Sexual Health Test
The Visby Medical Sexual Health Test is a POCT that enables result-driven, effective treatment delivery during a single clinic visit.
- It takes less than 30 minutes to process results from a patient-collected vaginal swab.
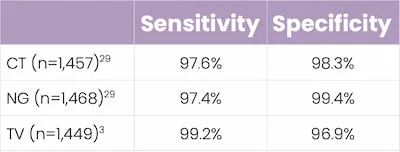
- It is a compact, single-use, disposable, nucleic acid amplification polymerase chain reaction (PCR) test that can test for and distinguish the genetic material of three pathogens causing chlamydia (CT), gonorrhea (NG), and trichomoniasis (TV).
- In studies, this POCT demonstrated high percent sensitivity and specificity across all three STIs.
Key Takeaways
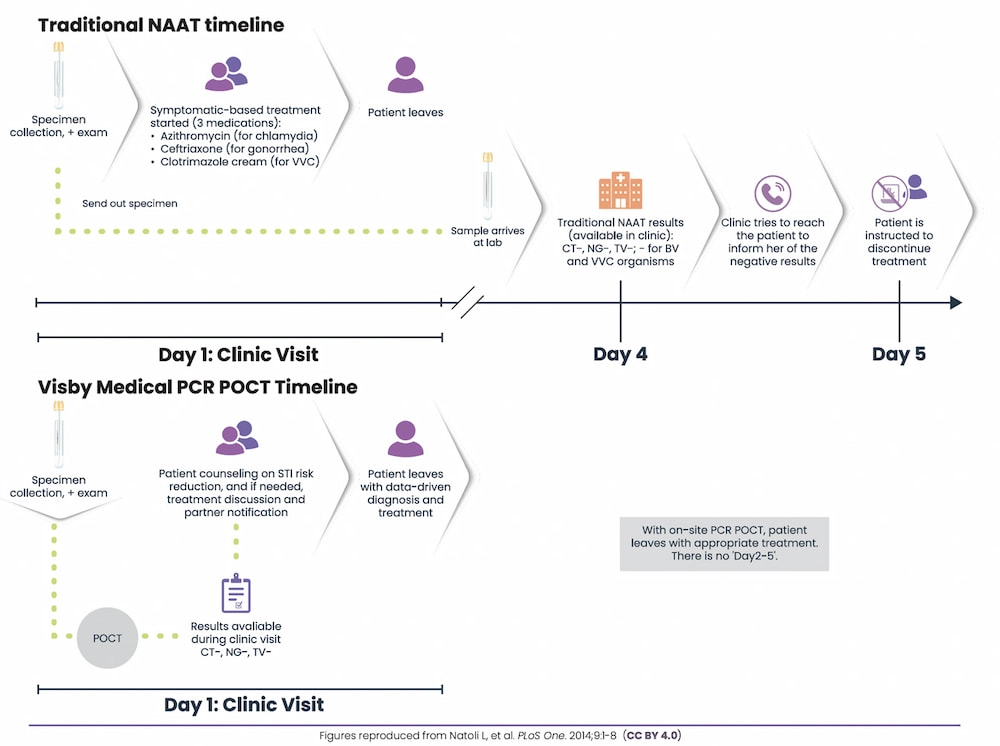
- Traditional PCR-based STI testing (e.g., lab-based NAATs) can take several days to return results; in this instance, syndromic management may be used to treat potential STIs.25,29
- Syndromic management of STIs can lead to both under- and overtreatment4
- Inappropriate use of antibiotics comes with risks
- Untreated STIs or failure to appropriately treat STIs increases the risk of complications, especially in women (e.g, pelvic inflammatory disease, infertility, ectopic pregnancy, miscarriage)2,44
- The use of POCTs allows a patient to receive an exam, precise diagnosis, STI education and prevention, and appropriate treatment all in one clinic visit. This helps expedite treatment for both the patient and their sexual partner(s) and reduce community spread.29,38

Traditional PCR/NAAT vs POCT38
References
- Dawkins M, Bishop L, Walker P, et al. Clinical integration of a highly accurate PCR point-of-care test can inform immediate treatment decisions for chlamydia, gonorrhea and trichomonas. Sex Trans Dis. doi: 10.1097/OLQ.0000000000001586.
- Sobel JD. Patient education: vaginal discharge in adult women (beyond the basics). UpToDate® website. Literature review current through October 2021. Updated March 8, 2021.
- Reno H, Park I, Workowski K, Machefsky A, Bachmann L. A guide to taking a sexual history. Centers for Disease Control and Prevention (CDC) website. Accessed November 3, 2021.
- Guidelines for the management of symptomatic sexually transmitted infections. World Health Organization (WHO) website. Published July 15, 2021. Accessed November 3, 2021.
- Huppert JS, Biro F, Lan D, Mortensen JE, Reed J, Slap GB. Urinary symptoms in adolescent females: STI or UTI? J Adolesc Health. 2007;40:418-424.
- Car J. Urinary tract infections in women: diagnosis and management in primary care. BMJ. 2006;332:94-97.
- How effective is the birth control pill? Planned Parenthood website. Accessed November 3, 2021.
- Copen CE. Condom use during sexual intercourse among women and men aged 15–44 in the United States, 2011–2015. Natl Health Stat Report. 2017;105:1-18.
- Speck PM, Faugno DK, Mitchell S, Ekroos RA, Hallman MG. Section 1: definitions and anatomical review. In: Sexually Transmitted Infection and Disease Assessment: for Health Care Providers and First Responders. STM Learning, Inc.; 2021:1-22.
- Mitchell H. ABC of sexually transmitted infections: vaginal discharge—causes, diagnosis, and treatment. BMJ. 2004;328:1306-1308.
- Syndromic management of sexually transmitted infections. Pan American Health Organization (PAHO) and World Health Organization (WHO) website. Accessed November 3, 2021.
- Coleman JS, Gaydos CA. Molecular diagnosis of bacterial vaginosis: an update. J Clin Microbiol. 2018;56:e00342-18.
- What is a urinalysis (also called a “urine test”)? National Kidney Foundation® website. Reviewed August 8, 2016.
- MedlinePlus. HCG in urine. Updated October 8, 2021.
- How to prevent sexually transmitted infections (STIs). The American College of Obstetricians and Gynecologists (ACOG) website. Reviewed August 2020.
- Azithromycin. DrugBank website. Updated November 3, 2021.
- Ceftriaxone. DrugBank website. Updated November 3, 2021.
- Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021;70:1-187.
- Clotrimazole. DrugBank website. Updated November 3, 2021.
- Leonard CA, Schoborg RV, Low N, Unemo M, Borel N. Pathogenic interplay between Chlamydia trachomatis and Neisseria gonorrhoeae that influences management and control efforts—more questions than answers? Curr Clin Micro Rep. 2019;6:182-191.
- Lovett A, Duncan JA. Human immune responses and the natural history of Neisseria gonorrhoeae infection. Front Immunol. 2019;9:3187.
- Markos AR. Chlamydia trachomatis genital infections. In: Markos AR, ed. Sexually Transmitted Diseases. Nova Science Publishers, Inc.; 2009:37-43.
- Garcia MR, Wray AA. Sexually transmitted infections. StatPearls Publishing. NCBI STATPEARLS website. Updated July 15, 2021.
- Gonorrhea – CDC fact sheet (detailed version). Centers for Disease Control and Prevention (CDC) website. Accessed November 3, 2021.
- Adamson PC, Loeffelholz MJ, Klausner JD. Point-of-care testing for sexually transmitted infections: a review of recent developments. Arch Pathol Lab Med. 2020;144:1344-1351.
- Pelvic inflammatory disease (PID) – CDC fact sheet. Centers for Disease Control and Prevention (CDC) website. Reviewed July 22, 2021.
- Caruso G, Giammanco A, Virruso R, Fasciana T. Current and future trends in the laboratory diagnosis of sexually transmitted infections. Int J Environ Res Public Health. 2021;18:1038.
- Clinic-based evaluation of point-of-care tests for the diagnosis of genital chlamydial, gonococcal, and trichomonas infection in women presenting with vaginal discharge. WHO Human Reproduction Programme (HRP) website. Final version July 22, 2016.
- Morris SR, Bristow CC, Wierzbicki MR, et al. Performance of a single-use, rapid, point-of-care PCR device for the detection of Neisseria gonorrhoeae, Chlamydia trachomatis, and Trichomonas vaginalis: a cross-sectional study. Lancet Infect Dis. 2021;21:668-676.
- Bowen VB, Johnson SD, Weston EJ, Bernstein KT, Kirkcaldy RD. Gonorrhea. Curr Epidemiol Rep. 2017;4:1-10.
- Antibiotics aren’t always the answer. Centers for Disease Control and Prevention (CDC) website. Accessed November 3, 2021.
- Kurowski K, Ghosh R, Singh SK, Beaman KD. Clarithromycin-induced alterations in vaginal flora. Am J Ther. 2000;7:291-295.
- Joseph RJ, Ser H-L, Kuai Y-H, et al. Finding a balance in the vaginal microbiome: how do we treat and prevent the occurrence of bacterial vaginosis? Antibiotics. 2021;10:1-39.
- Vaginitis. MedlinePlus website. Updated October 18, 2021.
- Gupta V, Sharma VK. Syndromic management of sexually transmitted infections: a critical appraisal and the road ahead. Natl Med J India. 2019;32:147-152.
- Toskin I, Murtagh M, Peeling RW, Blondeel K, Cordero, Kiarie J. Advancing prevention of sexually transmitted infections through point-of-care testing: target product profiles and landscape analysis. Sex Transm Infect. 2017;93:S69- S80.
- In-iw S, Braverman PK, Bates JR, Biro FM. The impact of health education counseling on rate of recurrent sexually transmitted infections in adolescents. J Pediatr Adolesc Gynecol. 2015;28:481-485.
- Natoli L, Maher L, Shepard M, et al. Point-of-care testing for chlamydia and gonorrhea: implications for clinical practice. PLoS One. 2014;9:e100518.